We are accepting patients on a waitlist. Availability is limited. Join our waitlist.
- Home
- / Blogs /
- PCOS
PCOS


When you’re a woman facing issues like weight gain, irregular periods, and strange hair growth, it’s tempting to think you can fix the problem yourself. But you may have polycystic ovarian syndrome (PCOS), a complex condition that affects between 5 and 10% of women of childbearing age. And although the symptoms presented by this concern may seem insurmountable, the team at Bloom La Vie Health in Liberty, MO, can help.
What Is the Main Cause of PCOS?
Roughly one in 10 women suffer from polycystic ovarian syndrome, caused primarily by an imbalance of reproductive hormones. The ovaries make and release an egg every month during a healthy menstrual cycle. But PCOS prevents the egg from developing or releasing as it should. For many women, the first clue they have this syndrome is difficulty getting pregnant (which can often be treated, but more on that later).
Outwardly, hormonal imbalances can cause such symptoms as:
- Missed, irregular, or very light periods
- Excessive body hair, including on the back, stomach, and chest
- Acne or oily skin
- Weight gain, particularly around the abdomen
- Thinning hair
- Skin tags on the neck or armpits
- Dark skin patches under the breasts, in the armpits, or on the back of the neck
- Understanding Androgens
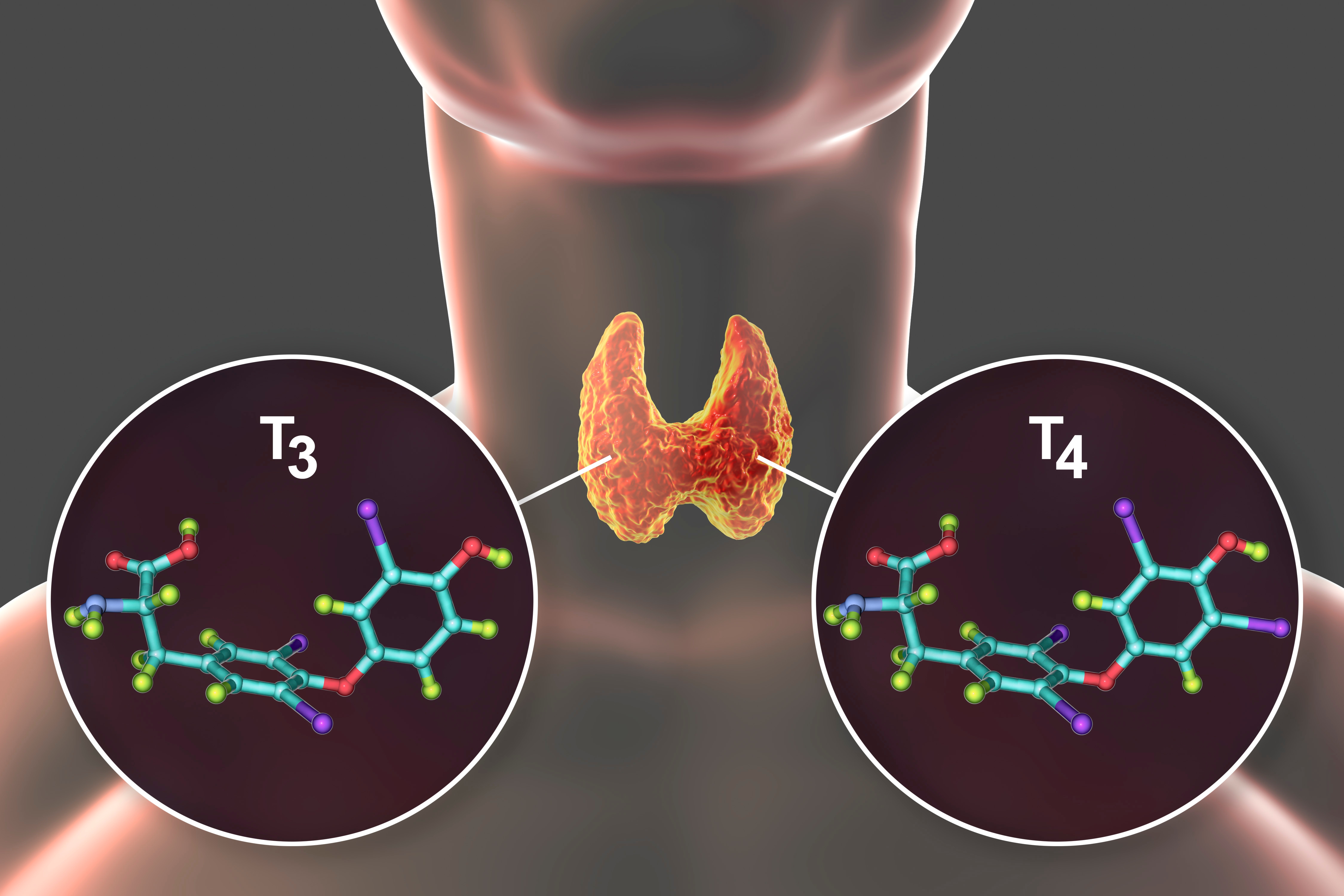
In addition to releasing eggs, the ovaries also produce hormones that manage reproduction. Among these are estrogen, often called the “female hormone” because women produce it in higher quantities than men, and androgens, conversely called “male hormones.” Males and females both need precise levels of these chemicals to maintain health.
All hormones must be kept in balance, but when it comes to reproduction, those produced in the ovaries are key. Women with PCOS have higher-than-normal levels of androgens that can disrupt estrogen and progesterone levels. The body strives at all times to keep these hormones delicately balanced, but sometimes, underlying factors stand in the way.
Traversing Muddy Waters
Let’s go back to our discussion of androgens, chemicals that we confess are not well understood. Some researchers suggest they may build up inside ovarian follicles and keep mature eggs from releasing. Others theorize they can interrupt brain signals that normally prompt ovulation.
But high androgen levels don’t necessarily lead to a diagnosis of polycystic ovarian syndrome. These hormones can fluctuate with many different health concerns, including Cushing’s syndrome. Doctors must therefore rule out other potential conditions before assuming excess androgens signal polycystic ovarian syndrome.
What Causes a Hormonal Imbalance?
On average, a woman sees three doctors and waits two years before learning she has this syndrome. A single test doesn’t conclusively prove PCOS, meaning a combination of ultrasounds, physical exams, and blood tests must instead be used. And because symptoms of this syndrome mimic those of other conditions, pinpointing the exact triggers of hormonal imbalance can be difficult and time-consuming.
Doctors have noted symptoms of polycystic ovarian syndrome since the 1700s. But well before this, Hippocrates (460 BC-377 BC) wrote of women with short periods and masculine appearances who did not become pregnant. Soranus of Ephesus (c. 98-138 AD) likewise observed some women never menstruated, and those who didn’t also possessed “manly” features and more robust statures.
Genetic Implications
These statements are suggestive of the same condition women today experience, giving rise to the belief that PCOS may be triggered by genes. A study from the University of Alabama at Birmingham confirms this theory; researchers found 24% and 32% of women with polycystic ovary syndrome had a mother or sister respectively diagnosed with the same condition.
The problem lies in understanding the precise role genetics plays. Experts previously believed a specific PCOS gene did not exist, but a 2019 meta-analysis published in The Journal of Clinical Endocrinology & Metabolism found that a gene called DENND1A may be responsible for this syndrome in white families of European descent.
Additional Family Traits
In families without the DENND1A gene – including those of African American heritage – a variety of mechanisms appears to be at work. This may explain the condition’s wide range of symptoms and why different women are affected at different ages.
Some experts further believe when fetuses are exposed to high levels of testosterone from their mothers, they may be more inclined to develop polycystic ovarian syndrome. Other research suggests this syndrome is a result of a person’s environment. For instance, lacking access to nutritious foods and maintaining a sedentary lifestyle can increase the likelihood of insulin resistance, which can further predispose a woman to polycystic ovarian syndrome.
Insulin Resistance
This brings us to our next point, which is the influence insulin holds over hormonal balance. The ins and outs of this chemical get a little tricky, so bear with us as we explain its relationship to reproduction. Your cells use insulin (another hormone) to absorb sugar from food and convert it into energy. The simplest way to explain insulin resistance is to say your cells don’t absorb sugar as they’re supposed to do.
This confuses your body into thinking more insulin is needed to compensate. Your pancreas then churns churn out increasingly higher levels of this hormone. High insulin levels can increase appetite and cause weight gain; they’re also indicators of prediabetes. Insulin resistance, meanwhile, can throw off ovarian activity and prompt the production of additional androgens, including testosterone. This male-dominant hormone is known to:= Produce dark patches on skin Contribute to stubborn weight gain Further disrupt estrogen and other hormones involved with normal ovulation
Luteinizing Hormone
One of the chemicals influenced by testosterone is luteinizing hormone, which completes crucial tasks throughout both halves of the menstrual cycle. In the first two weeks, this chemical is necessary to stimulate ovarian follicles to produce oestradiol. Around day 14, luteinizing hormone levels surge and prompt the ovarian follicle to tear and release a mature egg – the process known as ovulation.
In weeks three through four, luteinizing hormone stimulates the production of progesterone. This hormone is necessary to support the early stage of pregnancy if the egg released during ovulation is fertilized. It’s safe to say, therefore, that any factor known to disrupt luteinizing hormone levels can interfere with fertility.
A Look At Diagnosis and Treatment
At this point, you can probably see hormonal imbalances are far from simplistic. To reiterate, they can be triggered by a variety of factors that are difficult to single out. In addition, because an imbalance can be associated with many different conditions, clearly diagnosing a woman with polycystic ovarian syndrome isn’t an exact science. Overall, doctors look for at least two of the following symptoms:
- Irregular or absent periods
- Excessive face and body hair
- Hormonal acne
- Weight gain While different doctors will look for different combinations of symptoms, one general consensus does exist: a focus on treatment can help restore balance to a woman’s body. Bio-identical hormone replacement therapy (BHRT) is one such option that can be tailored to meet the needs of each patient individually.
Treatment with Progesterone
Bioidentical progesterone in particular can yield a variety of benefits in treating polycystic ovarian syndrome. This hormone signals the body to stop producing androgens, including the overproduction of testosterone. In time, the brain may develop the normal cyclic rhythm potentially disrupted in women with this syndrome. This can mean normal ovulation, regular periods, and restored fertility.
Progesterone receptors exist throughout the female body. Several studies suggest that in women with PCOS, cells that contain these receptors are progesterone resistant – meaning they don’t get the signals they need to properly function. Treating with BHRT can improve cell sensitivity and, as part of a holistic treatment plan, improve intrinsic hormone levels.
A Holistic Approach
What do we mean by a holistic treatment plan? Simply that traditional and non-traditional therapies can be combined to treat the root cause of polycystic ovarian syndrome. Traditional medicine tends to separate patients into segments, whereas holistic approaches consider your mental, physical, and emotional health to understand the whole of who you are.
For PCOS, we might recommend a plan that focuses on BHRT as well as diet, exercise, and supplements. For instance, we can arm you with the tools necessary to choose nourishing foods and engage in a level of activity that’s right for your body. This approach is much more effective than trying to treat your concern as an isolated incident.
Dispelling Myths
While the underlying cause of polycystic ovarian syndrome may never be known, we can assure you of one thing: you are not to blame. Once they receive a definitive diagnosis, many women think they could have done something to prevent it. But that’s oversimplifying the complex nature of this condition. As we explained earlier, a variety of factors – including genetics and environment – can influence the onset of this syndrome.
Other women think that losing weight will immediately reverse their condition. While stabilizing your weight will help balance your hormones, no immediate cure is known. We instead encourage you to make lifestyle changes to elevate your overall health. Nourishing foods and regular exercise, as mentioned earlier, can improve your body’s use of insulin. This can help balance other hormones and may be a first step in restoring healthy reproduction functions.
This Is a Rare Condition
Just the opposite, around 5 million women in the U.S. currently live with this condition. This marks it as one of the most common hormonal endocrine disorders in women of reproductive age. And data from the Polycystic Ovarian Syndrome Foundation suggests less than half of all women are diagnosed correctly when they present symptoms of this disorder, meaning millions of more women probably have it and aren’t even aware.
This Condition Prevents Pregnancy
Some women are still able to carry healthy babies to term. Before ruling out pregnancy, you must first give your body a chance and strive to balance your hormones. In addition, a variety of medications are available to stimulate ovulation. But even without these interventions, many women continue to ovulate intermittently on their own. Although this condition makes pregnancy harder, it’s not necessarily impossible.
Only Overweight Women Are Affected
While a number of women diagnosed with this condition are overweight, it affects ladies of all shapes and sizes. The connection between weight and PCOS is found in insulin; when the body can’t properly use this chemical, it’s easy to pack on additional pounds. This is why we recommend women establish a habit of healthy eating and regularly exercising.
Empower Yourself
The first step in managing this condition is obtaining a diagnosis. From there, we can provide the guidance you need to manage symptoms, balance hormones, and live a fuller life. Schedule your consultation today by calling Bloom La Vie Health in Liberty, MO.
Testimonials
What our patients say
Scroll through!I had such a lovely visit to Bloom La Vie Health! I am a little shy and the staff is so warm and welcoming! Was able to truly talk about what has been going on health wise and Dr. Nedeau listened!
Maddie
We moved the whole family to Bloom La Vie and have been so happy we’ve done so. Dr. Nedeau is so caring and knowledgeable, she listens to my concerns, and she has helped us navigate health issues so well.
Laura
So glad my husband and I moved to Bloom La Vie Health!! Her nurse Sandy and staff are so very caring and professional place to come! Also her Husband Joel keeps everything running smoothly!!!
Marie
Blog
Our Articles
Urgent Care
Sometimes life throws you a curveball and you need medical care when you weren’t expecting it. When that happens, Bloom La Vie Health in…
9787 N. Cedar Ave, Kansas City, MO 64157
(816) 408-3717
(816) 429-9762
support@bloomih.com

© 2025 Bloom La Vie Health. All Rights Reserved.
POWERED BY MODERN DOC MEDIA